Mental Health in Ghana
By Kayla & Grace
Mental health is a hot topic in the United States, with many organizations, like the National Alliance On Mental Illness (NAMI), working to de-stigmatize mental health disorders and provide support for patients and families. Nevertheless, mental illness is still a taboo subject in America, and many are suffering from inadequate access to healthcare. As Americans with interests in both healthcare and mental health—who also happen to have plans to travel to Ghana, it seemed natural to explore the topic prior to our arrival. We focus specifically on the attitudes surrounding the subject and the treatment methods utilized.
Tradition, Faith, and Biomedical Treatments
Access to mental health services is scarce on a global scale. In Ghana, only 2% of the population with mental illness has access to biomedical treatment. Traditional and faith healers (TAFH) are a key part of the mental health care system in low and middle income countries where patients with severe mental illness either do not receive formal psychiatric treatment. Because of uneven distribution of formal health care, TAFH serve as the first or alternative treatment for mental illness patients (van der Watt et al. 1). TAFH is perceived by the community as more accessible and affordable than formal health care and provide patients with culturally-relevant explanations to the cause of their illnesses (van der Watt et al. 2). Because of this, many Ghanaians rely on traditional and religious methods as treatment.
Perception of Mental Health
Mental Health in Ghana is understood to be directly related to spirituality or poor lifestyle choices. For example, excess drinking or drug use are often considered causes for abnormal behaviors resulting from mental health disorders like schizophrenia. A poor understanding of the underlying causes of mental illness allows for extreme stigma surrounding the issue. The mentally ill, their family members, and even those who provide them with medical care (e.g. nurses, doctors, etc.) “find it impossible to secure employment, housing, or a spouse” (Goldstone).
Treatments
One main mode of treatment is prayer camps. Here, families who have been cast aside and ostracized by society seek healing in the name of God. Sadly, these camps are not equipped to deal with mental illness in a productive way. When patients become violent, they are often restrained or caged (Goldstone). The prayer camps are not malicious in nature, and those running them are not necessarily to be blamed for the harsh conditions that are imposed. The real problem is the lack of resources available for Ghanaians dealing with mental illness(es).
Spirituality is believed to be the primary cause of mental illness according to prayer camp prophets (Ofori-Atta, A., et al. 6). According to prayer camp staff the main cause of mental illnesses are from demonic possession, and this can manifest in many ways. Demonic possession can show up from ancestral cursing, and substance abuse is said to be the manifestation of demonic spirit (Ofori-Atta, A., et al. 6-7).
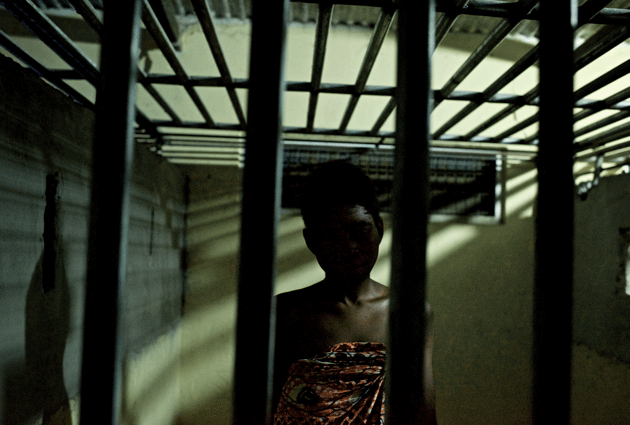
A prayer camp resident locked away due to a lack of solutions to the devastating problem of mental health.

The Nazareth Prayer Centre, in Akim Akroso.

What About Westernized Hospitals?
Ghanaians have a deep-seated mistrust for the country’s largest mental hospital. This facility is “[i]nfamous for its chaotic atmosphere and rampant abuse.” Additionally, even when mental health treatment is sought, it is not always helpful. For example, Veronica Donkoh was prescribed a “dangerous dosage of three antipsychotic drugs” when visiting a hospital in Kumasi. Veronica Donkoh suffers from schizophrenia, and has spent many years with her family hopelessly searching for a solid solution (Goldstone). It seems that when western medicine is utilized, it is not being harnessed in a productive way.
What’s Next?
There have been a multitude of unsuccessful attempts to remedy the situations in Ghana that we have presented, including passing the Mental Health Act. However, this piece of legislation “was not backed by a legislative instrument detailing how its protocols would be put into effect, or—most crucially—how its initiatives would be financed” (Goldstone). Sustainable, realistic, and accessible solutions must be found, as the current modes of treatment are not safe or helpful. The fact of the matter is that the western medicine introduced to Ghana is not helping. Furthermore, Ghanaians are reluctant to seek treatment in westernized hospitals due to the poor reputations of these facilities. A potential partnership that blends pharmaceuticals from the west with historically utilized Ghanaian treatment methods may provide some relief for suffering individuals.
Potential Partnerships.
According to Ofori-Atta, A., et al., prayer camps and biomedical staff are willing to partner together to combat mental illness. Prayer camps lack services for patients with severe mental illnesses and support biomedical education (Ofori-Atta, A., et al. 12). Disagreement between the two arise at the mention of long-term medication as a treatment (Ofori-Atta, A., et al. 13). Read suggests that Ghanaians are well aware of the availability of psychiatric drugs, but are not satisfied with long-term results due to uncomfortable side effects such as weakness and prolonged drowsiness (Read 451).
A Supplemental Solution?
A team at the University of Washington is currently working to develop resources for Ghanaians struggling with mental health problems. They propose an innovative mobile health approach utilizing the country’s advanced telecommunication system. They state,
Our team at the University of Washington is working with diverse stakeholders in the region (government officials, clinicians, NGOs, traditional and faith healers, people with mental illness and their communities) to develop mobile tools that leverage multi-media resources (video, audio) to combat stigma, introduce principles of humane care, and alternative strategies for psychosocial management of mental illness.
You can watch a video describing their work and vision here:
Concluding Statement
Originally, Kayla was looking at mental health treatments and Grace was looking at Ghanaian attitudes toward western medicine and were not sure how to connect these two ideas. Upon further research, they found that the lack of western medicine and psychiatric treatment has led Ghanaians to not only have limited access to biomedical treatment, but also to choose traditional and faith healers as the preferred method of treatment. Although traditional and religious treatments are not equipped to treat patients with severe mental illnesses, utilizing them in tandem with biomedical treatments has the potential to be very helpful.
References:
Goldstone, Brian, et al. “[Letter from Ghana]: A Prayer’s Chance.” Harper’s Magazine, 13 Apr. 2017, harpers.org/archive/2017/05/a-prayers-chance/.
“MHealth for Mental Health – The Case for Ghana.” mh4mh, The University of Washington, www.mh4mh.org/ghana.
Ofori-Atta, A., et al. “Joining psychiatric care and faith healing in a prayer camp in Ghana: Randomised trial.” The British Journal of Psychiatry 212.1 (2018): 34-41.
Read, Ursula. ““I Want the One That Will Heal Me Completely so It Won’t Come Back Again”: The Limits of Antipsychotic Medication in Rural Ghana.” Transcultural Psychiatry 49.3-4 (2012): 438-60. Web.
Van Der Watt, A., S. Van De Water, J. Nortje, T. Oladeji, G. Seedat, and B. Gureje. “The Perceived Effectiveness of Traditional and Faith Healing in the Treatment of Mental Illness: A Systematic Review of Qualitative Studies.” Social Psychiatry and Psychiatric Epidemiology 53.6 (2018): 555-66. Web.
Leave a Reply